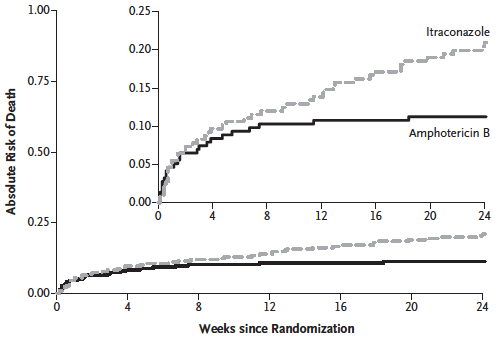
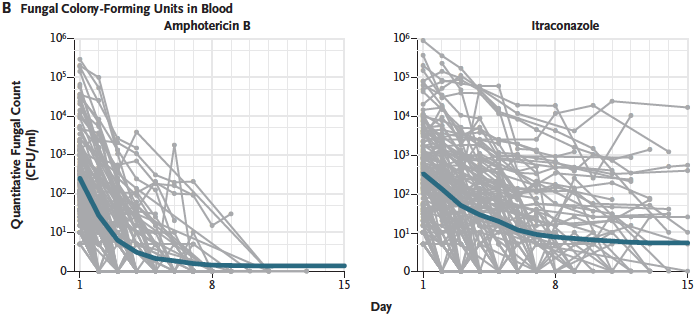
In a 440 patients study in Vietnam, Dr Thuy Le and colleagues show that conventional amphotericin B is superior to itraconazole for the treatment of talaromycosis in AIDS. Their paper published this month in the New England Journal of Medicine, finds not difference in 2 week mortality (6,2%), but a substantially higher mortality at 24 weeks in the itraconazole arm (21% vs, 10%). They also found a faster time to clinical resolution, more rapid clearance of blood cultures, and fewer relapses and episodes of immune reconstitution inflammatory syndrome (IRIS) in the amphotericin B arm.
Talaromyces (previously Penicllium) marneffei is the third most common AIDS-associated opportunistic infection in many parts of SE Asia. As a dimorphic fungus, it grows as a fission year in those with AIDS, usually causing skin lesions (80%) and positive blood cultures (70%). It is highly susceptible to both amphotericin B and itraconazole, and prior work showed itraconazole prophylaxis was effective at reducing infections. For this reason, and being oral. it was usually used as first line therapy to avoid the toxicities of amphotericin B.
In this study, the primary endpoint was 2 week mortality which did not differ, and had the authors done a short term study, the important clinical findings of a 10% improved 6 month survival would have been missed. The antifungal-attributable adverse events were higher in the amphotericin B group (infusion related reactions, anaemia, hypokalaemia, hypomagnesaemia and renal failure). However all serious adverse events (including poor control of infection, death and drug side effects) were more common overall in the itraconazole group (46% vs 27%).
Patients were enrolled from 5 hospitals in Vietnam over 3 years and 3 months, 135 per year. This suggests that the published estimate of an annual total of 206 cases in the country (Beardsley et al 2015) is a substantial under-estimate.
Article : AmB vs itraconazole for T. marneffei in AIDS RCT New Engl J Med 2017