Most prior work on Candida bloodstream infection incidence in the USA has been from small datasets with large specialised hospitals. In the MMWR, Mitsuru Toda and colleagues used a population of 8 million in 4 states (Georgia, Maryland, Oregon and Tennessee) to fully assess the contemporary situation of Candida bloodstream infections.
The crude annual incidence varied from 4.0 to 14.1/100,000, a mean of 8.7/100,000. As a country therefore with a population of 329 million in 2019 (UN figure), an expected 28,625 cases are expected annually, ranging from a low of 13,160 to 46,400. As blood culture is only 40% sensitive for invasive candidiasis, the relative incidence figures of IC are likely to be from 32,900 to 116,000 (mean 71,560 cases).
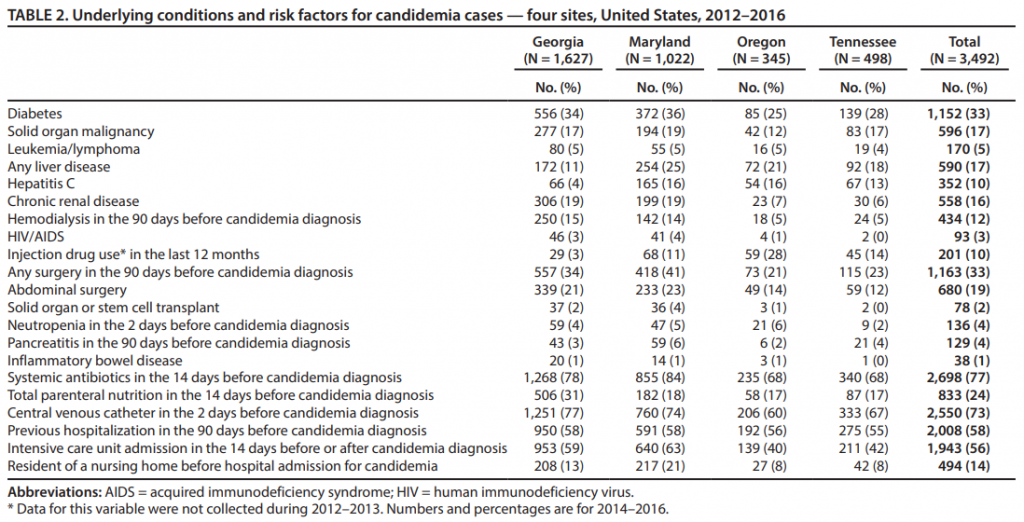
Amongst these cases a few remarkable findings emerge; 10% of cases are in IV drug abusers, 33% in diabetics and 17% in cancer patients. The relative rates in black people were double those of white people and males were slightly more often affected than females. Overall 23% had not received antibacterials in the prior 2 weeks, 86% had not had total parenteral nutrition and 27% did not have a central venous catheter in. Intensive care admission was required in 56% before or after the development of candidaemia.
Only 39% of cases were due to Candida albicans, confirming what is a long established trend in the USA for a preponderance of non-albicans species in candidaemia. C. glabrata was responsible in 28% of cases, C. parapsilosis in 15% and C. tropicalis in 9%: in 4% of cases multiple species were grown. C. auris was not detected. Overall 7% were deemed fluconazole resistant and 1.6% were echinocandin resistant.
Overall the in-hospital all cause mortality was 25%, lower than in many prior series.
Read the paper: Toda et al (2019)