Exposure to Histoplasma in the air is common in Guatemala (as in many other countries). In ASI ‘s* diagnostic program in collaboration with GAFFI, more and more patients tested positive for disseminated histoplasmosis as more samples were sent.
Narda Medina and colleagues report that in 2017, 1836 people with HIV infection were screened and 120 (6.5%) were positive for histoplasmosis, and by 2019, 202 were positive out of 2306 tested (8.8%).
Untreated, histoplasmosis in AIDS is nearly 100% fatal, so diagnosis is critical for survival. Histoplasmosis is often confused with TB. Optimal therapies are amphotericin B and itraconazole, both available in Guatemala. There are different formulations of amphotericin B and the liposomal formulation is superior to conventional (deoxycholate) amphotericin B, as shown in 2002 by Philip Johnson and colleagues. Liposomal amphotericin B was not available in Guatemala, but now is, thanks to GAFFI’s program.
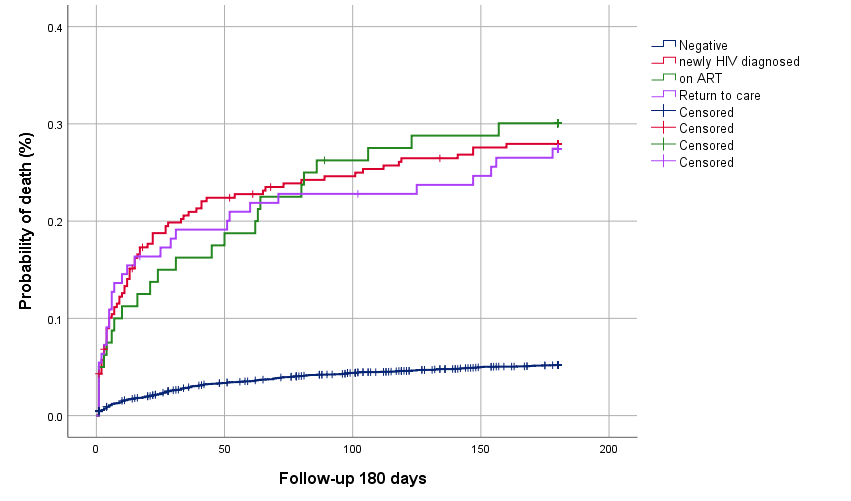
The mortality of those with histoplasmosis was similar regardless of whether newly diagnosed with HIV, on antiretroviral therapy (ART) or returning to care having discontinued ART. The incidence of the disease was about 40% lower in those taking ART. Nearly 16% of patients had dual or triple serious infections (usually TB or cryptococcosis), and this carries a worse outcome.
Histoplasma capsulatum concentrates and grows in nitrogen-rich soil, notably related to bat guano or bird excreta. The spores become airborne with soli disturbance and are breathed in, usually with little or no symptoms. But like TB, it persists in tissue for years (so-called latency), and can grow when the immunity wanes, as in advanced HIV disease (AHD) and after transplantation. Skin test surveys show variable rates of exposure by locality, but in Guatemala and many parts of Central and South America and the Caribbean exceed 60%.
* Asociación de Salud Integral, Guatemala City www.facebook.com/ASIGuatemalaONG/